What to Expect in the Last Stages of Acute Kidney Disease : 13 Signs and Symptoms of Death
Introduction
The last stages of acute kidney disease (AKD) are very emotional and complicated. It’s important to know what to expect, whether you’re a family member, caregiver, or healthcare worker. The decline in kidney function during AKD doesn’t just affect the kidneys; it affects the whole body and mind, and it often means that life is coming to an end. This guide is a kind and scientifically based resource that will help you see the important signs of this change, which will lead to more meaningful moments, better preparation, and a dignified goodbye.
Understanding the Final Phase of Acute Kidney Diseas
This article is about making people more aware of what happens when acute kidney disease gets worse. During these crucial hours or days, the body emits signals—physical, emotional, and psychological—suggesting that death may be approaching. Learning about these 13 signs can help families get better end-of-life care and get through this challenging time.
Important Benefits of Noticing These Signs
- Prepares family members mentally and spiritually
- Helps people make smart choices about hospice and palliative care
- Cuts down on unnecessary medical procedures and stress
- Makes patients more comfortable and dignified
- Encourages honest communication and closure
- Helps healthcare teams make sure that care is in line with what the patient wants and needs.
Recognizing these signs doesn’t mean losing hope; it means moving from medical treatment to care that is meaningful and centered on the person.
Myths, misperceptions, and Medical Facts
Some common myths are
- They’re just sleeping longer; they’ll be fine soon.
- Force-feeding might strengthen them.
- Dialysis can fix this, even now.
- Kidney disease always hurts when you die.
The Realities of Medicine
- Loss of consciousness, appetite, and urine output are all signs that an organ is shutting down.
- Extending life artificially may exacerbate suffering without enhancing quality.
- Hospice and palliative care teams are trained to help people feel less pain and less mental anguish.
- At this point, love, comfort, and being there for someone are the most important things.
How to Use This Information with Kindness
Make sure to talk to your healthcare providers regularly to find out what the prognosis is.
- Make the space calm by using soft lighting, familiar voices, and not too much stress.
- Talk to the patient softly, even if they don’t respond. Hearing is the last sense left.
- Focus on emotional support instead of medical help, unless it makes you feel better.
- Work closely with hospice or palliative care teams to make sure you get relief from physical, emotional, and spiritual pain.
- Add spiritual or cultural end-of-life rituals that give you comfort and meaning.
Research and scientific support
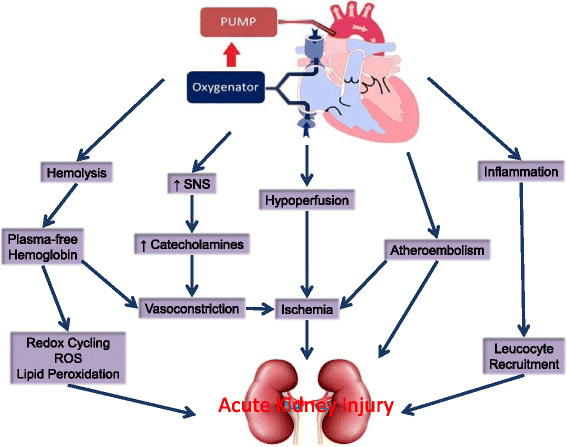
Peer-reviewed studies and hospice guidelines from the National Kidney Foundation, PubMed Central, and the Clinical Journal of the American Society of Nephrology indicate that these 13 signs frequently occur before death in individuals with acute or end-stage kidney failure. These signs show
- Dysfunction of multiple organs
- Increasing uremic toxicity
- Grave problems with electrolytes and metabolism
- Neurological decline caused by acidosis and toxin accumulation
Finding out about it early can make a big difference in how well families work together to care for their loved ones, manage their pain, and get closure.
Opinion of an Expert
“We shouldn’t be afraid of the signs of death; instead, we should see them as a call to love and care more deeply in the last moments.“
— Dr. Elaine Martin, MD, a specialist in palliative care
Her words remind us that knowing how to deal with death isn’t being cold and clinical; it’s being kind and knowledgeable.
Thinking about a real-life case
Razia Begum, a 72-year-old grandmother with advanced AKD, stopped talking and eating. Her family thought she was depressed. With the help of a palliative care nurse, they learned that these were normal signs of death. They didn’t push medical treatments; instead, they gave her warmth, prayers, music she liked, and a loving touch. Her children and grandchildren were with her when she died peacefully. Her journey wasn’t just a medical event; it was a holy end.
13 Signs and Symptoms of Acute Kidney Disease That Show Death Is Near
Here are the medically documented and emotionally significant signs to look for:
1. Extreme tiredness and weakness
Patients become bedridden and often can’t move or stay awake. As the body shuts down, it loses energy.
2. Hallucinations, confusion, and delirium
Uremia is the buildup of toxins that can alter your thinking, cause you to speak in unusual ways, or lead you to see deceased loved ones, which many consider a spiritual bridge.
3. No Urine at All (Anuria)
An epiphany transformed everything. The kidneys stop working completely. This phase is usually one of the last steps.
4. Severe edema causes swelling in the legs, hands, and face.
Swelling causes discomfort and can make it difficult to breathe because it retains fluid.
5. Breathing is hard or short.
Breathing is difficult, even when you’re not moving, because of fluid in the lungs and metabolic acidosis.
6. Throwing up and feeling sick a lot
Toxins upset the gut, which stops digestion. The patient might not even want water.
7. Uremic Breath (Smells Like Ammonia)
A strong, unpleasant metallic smell often comes from waste in the blood.
8. Severe Itching of the Skin (Uremic Pruritus)
If your skin is dry and irritated, it could cause open wounds. Itching happens when there is too much calcium and phosphate and too many toxins in the body.
9. The skin may appear pale, ashen, or have a yellow tint due to insufficient blood and oxygen supply to the body.
The skin tone becomes pale, gray, or waxy yellow because the body isn’t getting enough blood and oxygen.
10. No longer feeling hungry or thirsty
Anorexia at the end of life is the body’s way of saving energy. Making someone eat may make them upset.
11. Heartbeat that isn't regular or is slow
Potassium levels go up, which changes the heart’s rhythm. There is a chance of sudden cardiac events.
12. Patients may be unresponsive or in a coma.
Patients may not be able to wake up for hours or days. Even so, they might still be able to feel you.
13. Cold feet and mottled skin indicate circulatory shutdown.
Blood leaves the ends of the body, and blue spots may show up. This usually means that death is coming in a few hours or a day.
Conclusion and Call to Action (CTA)
The last stage of life is holy. It’s not just a time of loss; it’s also a time to honor, think about, and love. Understanding the 13 signs of death in acute kidney disease enables families to say goodbye with peace and clarity, ensuring a peaceful and respectful transition for the patient.
- Use this knowledge to help you choose presence over panic, love over fear, and meaning over medicine.
- If you found this guide helpful, please share it with others. Let people know about it. And if your loved one is about to take this last trip, know that you are not alone.
- Sign up for our newsletter to get more health guides that are kind.
- Get in touch with a local palliative care expert today to talk about your options for care.
Let’s take better care of each other, even at the end.
FAQs : Related Acute Kidney Disease
1. What are the signs that someone is dying from kidney failure?
In the last stage of AKD, you may feel awful, lose your appetite, be confused, not make any urine, have trouble breathing, have cold limbs, have mottled skin, and not respond. These signs mean that multiple organs are not working properly.
2. How long does a person live with acute kidney disease in its last stage?
It changes. Without dialysis or aggressive intervention, life expectancy in end-stage AKD is often from several hours to a few days, depending on overall health and medical care.
3. What happens in the last hours of kidney failure?
The patient might go into a coma, have cold hands and feet, have shallow breathing, not make any urine, and their blood pressure might drop. Hearing is usually the last sense left.
4. Is it possible for someone to get better after end-stage acute kidney failure?
At this point, recovery is very rare and usually not possible without immediate, aggressive treatment like dialysis and care in the ICU. This is often not recommended if the goal is comfort care.
5. Is it painful to die from kidney disease?
Not always. Medications can help with pain management when palliative care is done right. Supportive care may also help with emotional and spiritual pain.
6. When should you call hospice for someone who has kidney disease?
You should call hospice when the patient stops dialysis, their condition gets worse quickly, or they show signs of systemic failure, like confusion, coma, or organ shutdown.
7. What does mottled skin mean before someone dies?
Mottled skin, which looks like bluish or purplish patches on the hands or feet, means that the circulatory system is shutting down and is a common sign that death could happen within a few hours to a day.
8. What emotional signs do AKD patients show before they die?
Patients may become withdrawn, stop talking, cry easily, look scared, or say they are at peace. Your loved ones may see a change in your personality or openness to spirituality.
9. Should dialysis continue in end-stage renal failure?
Dialysis only makes things worse for most people who are dying, and it may not even improve their lives. It’s best to get advice from both the nephrology and palliative teams.
10. What are the spiritual signs that someone with kidney failure is about to die?
Some patients say they see dead relatives, feel a “presence,” or ask for prayer. Many people see these as signs of a spiritual change.
11. Is it possible for someone in a coma from kidney failure to hear?
Yes, hearing is usually the last sense to go. Your voice and kind words may bring them peace in their last moments, even if they can’t respond.
12. How do you make a kidney patient who is dying at home feel better?
- Keep them warm and clean.
- Play music, you know.
- Talk to each other in a kind and loving way.
- Give them ice chips to help with dry mouth.
- Get help from hospice for pain management.
- Concentrate on being there, being calm, and giving emotional support.
13. What does uremia do to the brain before death?
Uremia makes toxins build up in the body, which can lead to confusion, agitation, delirium, and even coma. It has a giant effect on brain function in the last stages.
14. Is it normal to stop eating and drinking when you die?
Yes. Not wanting to eat is a normal part of dying. It can be uncomfortable or harmful to force someone to eat or drink. Give them small sips only if they help.
15. What does palliative care do for people with kidney failure?
Palliative care:
- Handles physical signs
- Provides emotional and spiritual help
- Helps families make smart decisions
- It enhances comfort and respect during the final stages of life.
16. How can you prepare for the death of a loved one due to AKD?
- Talk about your feelings and what you want.
- Spend time together that matters.
- Get help from a counselor or a spiritual leader.
- Say what you need to say: love, forgive, and be thankful.
- Preparation lessens regret and makes the last moments more meaningful.
17. Would it be possible to manage pain in end-stage kidney failure without dialysis?
Yes. Hospice care can help with pain, nausea, shortness of breath, and anxiety by using medications that don’t hurt and other comfort measures.
18. How do you talk to a person who is dying and has kidney failure?
- Speak clearly and softly.
- Don’t talk about medicine.
- Talk about memories.
- Tell them that you love them.
- Your words have emotional weight, even if they don’t respond.
19. What part does staying hydrated play in the last stages of kidney disease?
Too much water can cause fluid to build up, making it harder to breathe. Unless it makes you feel better, it’s usually best to drink as little as possible.
20. Is it possible for final-stage kidney failure to be peaceful and painless?
Yes, with compassionate care, emotional support, and symptom management, patients can die peacefully, surrounded by loved ones, without any extra pain.